The Growing Weight of NCDs: Why India Can’t Afford to Ignore Chronic Illness Anymore

In India today, many people feel healthy — until one day, they don’t. A routine check-up reveals high blood pressure. A little fatigue turns out to be diabetes. A bit of weight gain hides a fatty liver condition. More and more Indians are living with health problems they can’t see, feel, or even suspect — until it’s too late. This is the reality of non-communicable diseases (NCDs), and it’s becoming India’s biggest health challenge.
A new study by Apollo Hospitals paints a sobering picture. Based on data from over 2.5 million people, the report warns that India is sitting on a silent epidemic. Conditions like diabetes, hypertension, fatty liver disease, and even depression are becoming common across all age groups, and many of those affected don’t even know it.
Take fatty liver disease, for instance. It’s often dismissed as a minor issue, but when left unchecked, it can develop into cirrhosis or even liver cancer. The Apollo study found this condition to be alarmingly widespread, with most cases going undiagnosed until advanced stages. That’s just one example of how NCDs work — slowly, silently, and dangerously.
Diabetes, too, is no longer a disease of old age. People in their 30s and 40s — sometimes even younger — are being diagnosed with high blood sugar levels. Even more concerning is the number of people who are in the pre-diabetic stage. They may not need medication yet, but without lifestyle changes, they’re walking a thin line toward long-term complications like kidney disease, nerve damage, or heart failure.
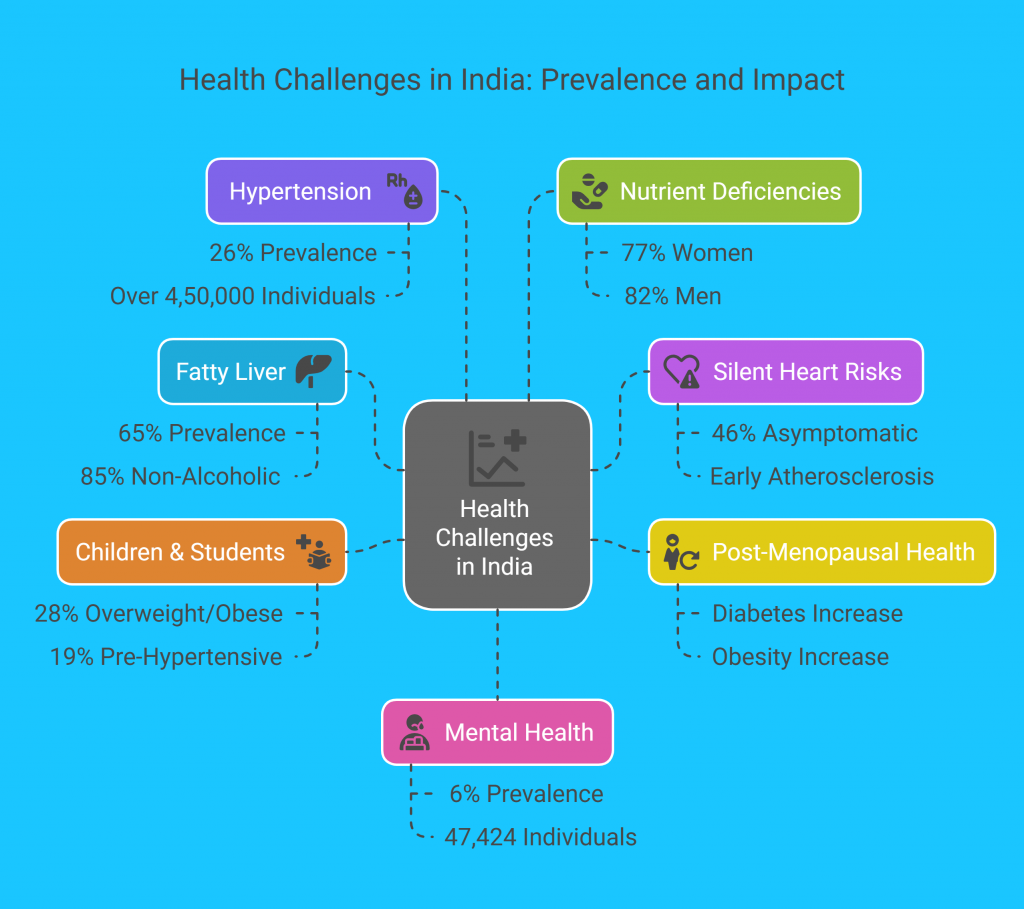
Key findings
Fatty Liver – 65% of 257,199 screened had fatty liver; 85% were non-alcoholic.
Silent Heart Risks – 46% of asymptomatic individuals had signs of early atherosclerosis
Post-Menopausal Health – Diabetes jumped from 14% to 40%; Obesity rose from 76% to 86%.
Children & Students:- 28% of college students overweight or obese; 19% are pre-hypertensive.
Hypertension – Found in 26% of over 4,50,000 individuals.
Nutrient Deficiencies: 77% of women and 82% of men had Vitamin D deficiency.
Mental Health: 6% of 47,424 individuals screened showed signs of depression.
Sleep Disorders (OSA) : 24% of 53,000 screened were at high risk of Obstructive Sleep Apnea (OSA).
Hypertension, or high blood pressure, is now being seen in younger age groups as well. It rarely shows symptoms in its early stages, yet it quietly increases the risk of stroke and heart attack. Then there’s the issue of mental health — the stress, anxiety, and depression that often go unnoticed but can deeply affect physical health too.
So what’s driving this surge in chronic illnesses?
A lot of it comes down to how we live today. We move less, sit more, eat more processed food, and deal with more stress than ever before. Urban life, while full of opportunity, comes with long work hours, screen addiction, and irregular routines. Even in smaller towns and rural areas, lifestyles are changing — fast food is no longer a city phenomenon, and physical activity is on the decline.
There’s also a cultural gap when it comes to preventive healthcare. Regular check-ups are still not a priority for most people. Many only visit a doctor when something feels seriously wrong — and by then, the disease has often progressed. This delay in diagnosis is a major reason why NCDs are so difficult to manage once detected.
But the good news is: most of these diseases are preventable, or at least manageable, with timely action.
The Apollo report makes it clear — early detection is key. That means going for health screenings even when you feel fine. That means paying attention to small signs: tiredness, changes in weight, sleep issues, stress levels. These could be your body’s way of warning you.
The bigger picture also calls for a shift in how we, as a country, think about health. Public campaigns can help people understand that NCDs are not just “lifestyle” diseases — they’re serious medical conditions that deserve attention. Access to affordable screenings, especially in underserved communities, can help catch problems early. Schools, workplaces, and local communities can do their part by encouraging better nutrition, regular activity, and mental well-being.
Policy changes matter too. Clearer food labeling, urban infrastructure that supports walking and cycling, and support for wellness programs can all help build a healthier environment. But real change begins at the individual level — choosing to move more, eat better, manage stress, and prioritize routine check-ups.
India’s health story is at a turning point. We’ve made great strides in controlling infectious diseases. But now, it’s time to turn our focus to the long-term, slow-burning threat of NCDs. These aren’t diseases that make headlines overnight — but over time, they cost lives, drain families, and burden the healthcare system.
The Apollo Hospitals study is a wake-up call, not just for policymakers and doctors, but for all of us. It’s a reminder that staying healthy isn’t just about avoiding illness — it’s about actively building habits that protect us in the long run.
The epidemic may be silent, but the response doesn’t have to be. It’s time we started listening — to the data, to our bodies, and to the growing urgency of India’s chronic illness crisis.