The Growing Burden: Obesity in Indian Women Is Starting Younger Than Ever

A silent epidemic is unfolding in India. It isn’t sudden or dramatic. It builds over time, reshaping the health of millions of women. Obesity, once linked mostly to the West, is now a growing concern across India. Women, both in urban and rural areas are increasingly being affected. And it’s starting young.
Recent studies reveal that more than half of Indian women between the ages of 18 and 30 are already overweight or obese. These figures represent a major shift from trends seen a generation ago. The consequences go far beyond appearances. Obesity is now recognised as a significant barrier to health, especially for women of reproductive age.
A new consensus published in the Indian Journal of Obstetrics and Gynecology Research focuses on this growing concern. Led by a panel of 12 experts nationwide, the paper outlines clinical guidelines for managing obesity in women. It particularly addresses women who are planning a pregnancy or undergoing fertility treatments.
The Indian Society of Assisted Reproduction developed the statement. It is based on insights from over 75 studies and health surveys, including the National Family Health Survey and global public health data. It offers structured advice for doctors, but its core message is clear: obesity in Indian women demands urgent public health action.
National-level data confirms that this issue is widespread. According to NFHS-5 (2019–21), 33.2% of urban women and 19.7% of rural women in India are overweight or obese. This is defined as having a BMI greater than 25. These rates are no longer confined to wealthier or urban households.
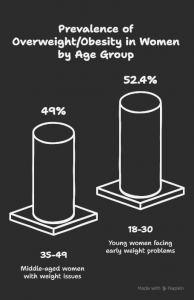
Obesity also rises with age. In a study covering over 6.4 lakh women, nearly 49% of those aged 35 to 49 were found to be overweight or obese. Alarmingly, a separate study found that 52.4% of women aged 18 to 30 were already in this category. This data signals a shift in the age at which weight-related health issues begin.
The health implications are serious and multi-faceted. Obesity is linked to a range of medical conditions that particularly affect women. These include irregular periods, infertility, Polycystic Ovary Syndrome (PCOS), gestational diabetes, and high blood pressure during pregnancy. It also increases the likelihood of miscarriages, stillbirths, birth complications, urinary incontinence, and fibroids. The risk of C-sections is higher in obese women.
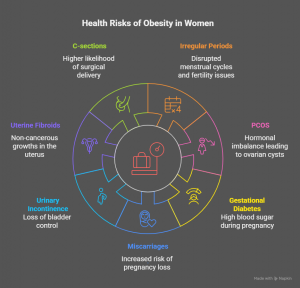
These conditions do not occur in isolation. They often cluster together, making long-term health management even more challenging. For many women, problems begin as early as puberty and persist through menopause. Obesity is also known to worsen mental health conditions, and increases the likelihood of cardiovascular disease and metabolic disorders later in life.
To tackle this, the consensus calls for early detection and regular monitoring. It recommends that doctors assess body weight, waist circumference, and lifestyle factors during routine check-ups. This is particularly important for women planning to conceive, as obesity is now one of the leading preventable causes of infertility.
One encouraging insight from the research is that even small changes can have a big impact. Losing just 5 to 10% of one’s body weight can significantly improve hormonal balance. It can also help restore ovulation, reduce insulin resistance, and increase the chances of both natural conception and IVF success. Women with PCOS have seen improvements in menstrual regularity and reduced risk of miscarriage after modest weight loss.
The benefits of weight loss go beyond fertility. It improves mobility, reduces urinary issues, and boosts mental well-being. These changes contribute to a better overall quality of life and lower risk of chronic illnesses over time.

The recommended approach to managing obesity begins with lifestyle changes. These include cutting back on sugary foods and saturated fats, eating more protein and fiber, exercising for at least 150 minutes each week, and maintaining good sleep hygiene. Mindful eating and portion control are also critical for long-term success.
Psychological support can be helpful as well. Cognitive Behavioural Therapy (CBT), for example, has been shown to help individuals address emotional eating and stay motivated. When lifestyle changes alone are not enough, medical intervention may be considered. This is typically advised for women with a BMI over 27 and a related condition, or for those with a BMI over 30.
Currently, Orlistat is available in India. Another medication, Semaglutide, has been approved by Indian regulators but is not yet widely accessible. Both have shown promising results in clinical trials, including improved hormone levels and fertility outcomes. However, these drugs should not be used during pregnancy or breastfeeding.
In cases where obesity poses serious health risks, bariatric surgery may be considered. This option is generally for women with a BMI over 35 or who have significant complications. Surgery has been shown to improve fertility and reduce pregnancy-related risks. However, doctors recommend waiting at least 12 months post-surgery before trying to conceive.
For women who are already pregnant, medications are not recommended. Instead, focus is placed on diet and physical activity. Managing weight gain during pregnancy is important. Postpartum, structured programs that aim for slow and steady weight loss—about half a kilo per week—are suggested.
Breastfeeding plays a key role in postnatal weight management and should be encouraged. Once breastfeeding ends, medications can be discussed with a doctor if needed. For women in their 40s and 50s, the focus should shift to monitoring muscle and bone health, and screening for diabetes and heart disease.
The consensus statement also includes trimester-specific weight gain guidelines. These aim to reduce complications and support healthy pregnancies. Postpartum care is equally important and should include physical activity, dietary support, and mental health resources.
Obesity among Indian women is not about image or personal choices. It is a complex health issue that affects fertility, mental health, pregnancy, and long-term well-being. The new recommendations provide a roadmap for doctors. They also reflect a shift in how society must view women’s health—not just as a reproductive issue, but as a lifelong continuum of care.
Addressing obesity isn’t only about reducing numbers on a scale. It’s about giving women the chance to live fuller, healthier lives.